Disease
Autoimmune Hepatitis
1. What kind of disease is it?
Autoimmune hepatitis is hepatitis that, in many cases, progresses to chronic disease and damages liver cells. A blood test will indicate that the blood levels of AST and ALT have risen to the extent that liver cells are damaged. It is believed that immune abnormalities are related to the onset of autoimmune hepatitis. The disease is characterized by prevalence in females who are middle-aged or older. It is diagnosed when liver disorders with clear causes, such as the hepatitis virus, alcohol, drug-induced, and other autoimmune diseases, are ruled out. Corticosteroids are effective in the treatment of the disease. The name of the disease, autoimmune hepatitis, is abbreviated to AIH.
2. How many people are affected by this disease?
A survey conducted by our study group in 2004 estimated that there were approximately 9,000 patients throughout Japan (9 in 100,000 people). The survey was repeated in 2018, and this time the estimated number of patients throughout Japan was 30,000 (24 in 100,000 people). This would indicate that over 14 years, the number of patients with AIH approximately tripled.
3. What sort of people are susceptible to this disease?
The male-to-female ratio for patients diagnosed with autoimmune hepatitis is 1:4, with more females suffering from the disease. Many female patients are middle-aged (in their fifties and sixties), but it is not unusual for young women and children to develop the disease. The trend in recent years has been toward higher numbers of male patients than in the past and for older people to develop the disease.
4. Are the causes of this disease known?
The cause is unknown. As blood tests show positive results for autoantibodies (antinuclear antibodies, anti-smooth muscle antibodies), high immunoglobulin and IgG levels, and that patients are often responsive to corticosteroid treatment, it is believed that autoimmunity is involved. Liver tissue testing reveals the presence of high numbers of lymphocytes in the liver and liver cell damage. In some cases, the disease develops due to viral infection, drug administration, or following pregnancy and childbirth. It has been reported that these factors may be triggers of disease onset.
5. Is this disease hereditary?
Although it is not genetically transmitted, 60% of Japanese patients are positive for HLA-DR4, and many patients in Europe and the United States are positive for HLA-DR3 and HLA-DR4. This suggests the involvement of some genetic factor in disease onset. However, unlike PBC, no clear gene related to AIH onset has been found. Although there have been cases of an outbreak among parents and children, and siblings, these are extremely rare.
6. What are the symptoms of this disease?
Typically, there are no subjective symptoms, and therefore, in many cases, the disease is discovered incidentally during regular health examinations. Some people complain of symptoms such as systemic fatigue, tiredness, and poor appetite. In cases of acute hepatitis, symptoms include fatigue, jaundice, and poor appetite, but autoimmune hepatitis has no characteristic symptoms. It is sometimes discovered after having progressed, and once the disease has progressed to cirrhosis of the liver, symptoms such as swelling of the lower extremities, swelling of the abdomen due to ascites, and bloody vomit (hemorrhaging from esophageal and gastric varices) can occur.
Topic (1): Acute hepatitis-like AIH
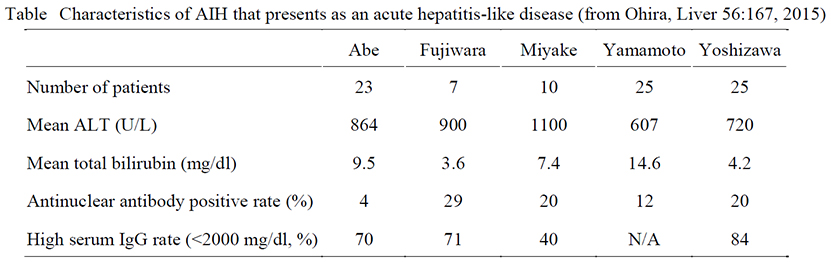
Normally, AIH appears as acute hepatitis, there are almost no symptoms, and in many cases, it is discovered through incidental blood test results. However, some patients experience symptoms such as systemic fatigue and jaundice as well as sudden disease onset. In many cases of acute hepatitis-like disease onset, the characteristics of AIH, such as positive for antinuclear antibodies and high serum IgG levels, are not found, and as a result, it is often difficult to diagnose a patient with AIH. This then leads to delays in corticosteroid treatment, during which time hepatitis may progress, and in some cases, patients can even die of fulminant hepatitis and acute liver failure. Currently, we are working to create diagnostic criteria that will allow us to diagnose AIH, which presents as an acute hepatitis-like disease in its early stages and begin treatment earlier.
7. How is this disease treated?
The basic treatment is the administration of immunosuppressive drugs, the first of which is the oral drug corticosteroid. One of these drugs, known as prednisolone, is administered at disease onset at a dose of between 30 and 40 mg per day (when the disease is severe, between 50 and 60 mg per day). Once this leads to improved liver function levels, the prednisolone dose is gradually reduced to between 5 and 10 mg per day with eventual transition to another drug as the goal. The objective of treatment is to return liver function levels, especially ALT and IgG, to normal. Either from the start of treatment or while the prednisolone dose is being reduced, another drug called azathioprine is sometimes administered in doses ranging from 50 to 100 mg per day. This allows the prednisolone dose to be reduced earlier or discontinued in some cases. However, once both corticosteroid and azathioprine are both completely discontinued, autoimmune hepatitis recurs and liver function levels worsen again in many cases. This requires a maintenance dose over the long term of either prednisolone or azathioprine at the minimum required dose to maintain stable levels. In cases in which the disease recurs while drug doses are being reduced or during the maintenance dose administration period, corticosteroid dose increases and combined administration of azathioprine are considered.
Adverse drug effects that may occur during corticosteroid administration include peptic ulcer, moon face, diabetes, dyslipidemia, and osteoporosis. Although azathioprine has relatively few adverse side effects, the white blood cell and platelet counts may suddenly decrease. These adverse side effects are well-understood, and thus patients need to be administered preventative drugs in accordance with their condition. Middle-aged and older females have a particularly high risk of developing osteoporosis, and thus they should undergo regular bone density tests. If a decrease in bone density is discovered, drugs to improve their bone density must be administered. If patients decide on their own to discontinue immunosuppressive drugs such as corticosteroids and azathioprine, autoimmune hepatitis may recur, and thus it is important for patients to closely follow their drug regimen.
Topic (2): Novel drugs other than prednisolone and azathioprine
Prednisolone is an extremely effective drug, but it is known to have many adverse side effects. Azathioprine also has adverse side effects that cannot be ignored, and thus some patients are unable to take either of these drugs. These AIH patients require immunosuppressive drugs other than prednisolone and azathioprine. In Europe and the United States, an corticosteroid known as budesonide, which mitigates adverse side effects, and a different type of immunosuppressive drug known as mycophenolate mofetil are used. Although these drugs are insufficient, their therapeutic effects are currently being confirmed. We are planning to continue research in the future in the form of clinical studies and trials with the cooperation of patients and pharmaceutical companies so that budesonide and mycophenolate mofetil can someday be utilized in Japan.
8. What is the course of this disease?
Since disease onset is prolonged and the subjective symptoms are often mild, the patient does not typically notice disease onset. As a result, the disease is frequently discovered and diagnosed incidentally through a medical checkup. However, disease progression is swift if allowed to go untreated, and it is not unusual for the disease to progress from liver cirrhosis to liver failure. Most patients who undergo appropriate treatment show rapid improvement in the inflammation of the liver and cessation of disease progression. A survey conducted in Japan found that the long-term prognosis for patients with AIH who underwent appropriate treatment and whose liver functions stabilized is good and that their mortality rate is the same as that for the general population. However, some patients whose liver function tests frequently show poor results have a poor prognosis, and some of these patients develop liver failure or hepatocellular carcinoma.
9. What precautions in daily life are required?
Corticosteroids are used to treat AIH, but the adverse side effects of this drug include increased appetite, obesity, diabetes, and dyslipidemia. Therefore, patients must be careful about the amount they eat, avoid high caloric intake, and make sure they do not gain weight. In cases in which a patient is taking relatively large doses of prednisolone (at least 15–20 mg/day), they should wear masks when in crowded areas and avoid locations with large amounts of dust to lessen infection risk by some pathogen. On the other hand, if they are taking maintenance doses of prednisolone (5-10 mg/day), no particular precautions, including those against infection, are required, and they may work and travel without restrictions.
Patients may be vaccinated with inactive vaccines (e.g., influenza, pneumococcus, hepatitis B) and toxoid vaccines (e.g., diphtheria, tetanus). Vaccines may have reduced preventative effects while a patient is taking immunosuppressive drugs such as corticosteroids. However, since there is a risk that they may develop severe symptoms because of the immunosuppressive drugs if they were to be infected with influenza or another disease, it is recommended that patients are vaccinated. On the other hand, patients taking corticosteroids or immunosuppressive drugs are generally unable to be administered live vaccines (e.g., measles, rubella, mumps).
AIH often subsides during pregnancy, but following childbirth can worsen, and liver function test results can become elevated. In such cases, the patient should consult with their attending physician and obstetrician. It is believed that doses of corticosteroids between 5 and 10 mg per day do not affect pregnancy and childbirth. Azathioprine is not generally recommended to be taken during pregnancy. Nevertheless, as it is known to be relatively safe, in July 2018, it was approved for use when necessary on pregnant women.

